We are starting a new blog-series related to the key-methodological aspects concerning the introduction of new digital solutions. In this first blog, we raise issues as to why we as an industry, need to engage in order to support the creation of better frameworks.
We recognise that there is great potential in the use of digital health. Equally, I think we understand that there are many digital initiatives that lack value. In the context of our blog-series, the scope covers solutions that have a therapeutic, diagnostic, or major role in the management of disease.
In our review of digital health readiness across western European countries, we have not found any country that provides a holistic framework to support the introduction of relevant digital solutions. Obviously, there are elements in place in most countries. We would still suggest that the lack of structure and process is a major concern. Many may consider this ‘freedom’ as valuable, we would argue otherwise.
Why should industry care if there is a poorly regulated process to introduce digital health solutions?
- Significant amounts of money are wasted on projects which have no or limited benefit.
- Solutions that could bring savings to healthcare are not introduced.
Both aspects have significant implications for the overall availability of the health care budget. Wasted money in this area will lead to less money for valuable drugs and interventions.
In this blog-series we will discuss what we consider to be the main methodological issues that would be considered essential to ensure beneficial utility of digital health in our health care systems.
Selecting the areas of relevance to consider – What is the minimum threshold of the value of a digital solution?
The value of digital solutions will either come from a change in how care is organised or from a changed behaviour by the patients. Either of these will generally require an intentional change process to ensure successful implementation. With scarce resources to support such change, it is crucial to implement solutions that are the most impactful and ensure they are well implemented.
This is an interesting example from Denmark regarding COPD when they first evaluated the potential benefit of digital solutions in combination with the required effort to implement this on a national level.
In the below graph from the report they show the cost to implement and run the services and how the cost-saving will evolve over time. Eventually, it will lead to an annual saving of 200 million DKK / year.
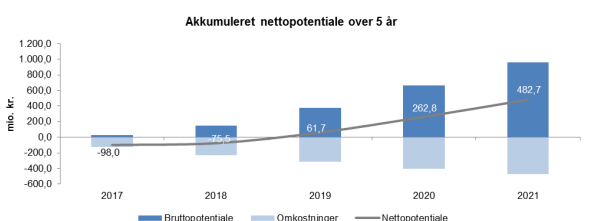
Business Case (see page 8)
Conceptually, we would suggest that countries would benefit from defining the thresholds for when it is worth implementing a digital solution. This could either be on a generic level or for a specific disease.
Conceptually we would suggest a model like this:
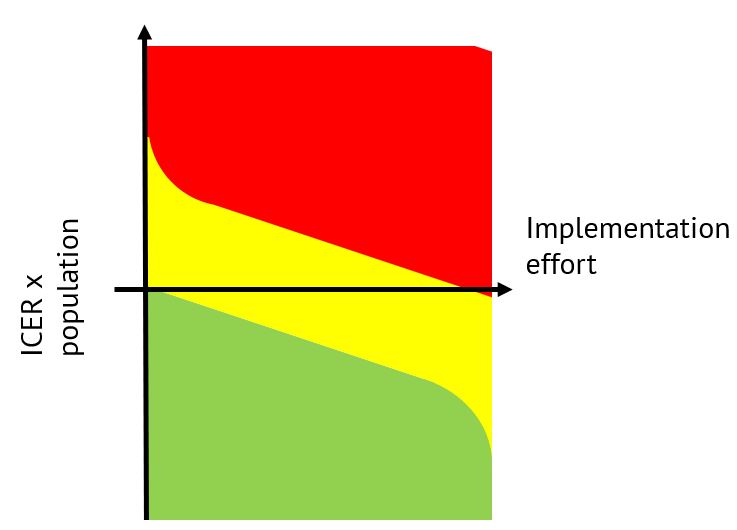
On the y-axis, you have the incremental cost-effectiveness ratio multiplied with the applicable population. The focus is on solutions that can bring more value for the money with a large impact.
The x-axis represents the effort to implement the solution. There are solutions that can provide a rather small saving but have a limited effort for implementation and therefore should be implemented, whereas there are others that will require a substantial effort but also provide a more significant return.
In the consequent blogs, we are going to address the following topics:
- Selecting the right solution in the basket of options
- Methods to evaluate the effectiveness
- Implementation support
- Payment mechanisms
Note:
- For further updates on this blog-series, please join the LinkedIn group (Digital Health Market Access) where we look forward to your feedback as we share more insights.
- Feel free to also comment on the LinkedIn post.


